Introduction
Although epilepsy and psychiatric disorders are discrete disease entities, comorbid psychiatric disorders are commonly observed in patients with epilepsy (PWE).1 Landolt described a characteristic group of PWE who showed the occurrence of long-lasting psychotic state after normalization of electroencephalography (EEG) and named this phenomenon as “forced normalization (FN)”.2 It has been controversial whether this phenomenon truly exists or not. Herein, we report the case of a patient who showed a long duration of first-onset psychiatric symptoms after remission of seizures and normalization of EEG, which is compatible with the phenomenon of FN and discuss the possible pathomechanisms.
Case Report
A 41-year-old male visited the Department of Neurology because of poor control of seizures. He had been diagnosed with epilepsy 14 years prior. His seizures were poorly controlled despite the administration of anti-seizure medications (phenytoin 100 mg twice a day), and he had four to five seizures per month. Regarding his medical history, he had a motor vehicle accident and traumatic cerebral hematoma 15 years before the visit. His family members and caregivers reported no other past medical history or family history of psychiatric illness. However, he had had a moderate depressive mood and intermittently showed impulsive behavior since the head injury. Almost all of his seizures had been during sleep. He denied any prodromal symptoms or aura before seizures. Generalized tonic-clonic seizures following grunting sounds had been noticed by caregivers during every ictal period.
Computed tomography revealed cerebromalacia in the right frontal area (Fig. 1A). The initial EEG revealed frequent epileptiform discharges in the right frontal leads (Fig. 1B). We initially administered valproate 500 mg twice daily; however, the seizures persisted. We gradually decreased the dose of valproate and changed it to topiramate, which was initiated at 25 mg twice daily and gradually increased to 100 mg twice daily for 2 months.
Figure 1.
(A) Computed tomography showed cerebromalacia in the right frontal area (black arrow). (B) Electroencephalogram revealed frequent epileptiform discharges in the right frontal leads (arrows). (C) Follow-up electroencephalogram showed the disappearance of preexisting epileptiform discharges. Fp, frontopolar; F, frontal; C, central; P, parietal; O, occipital; T, temporal.
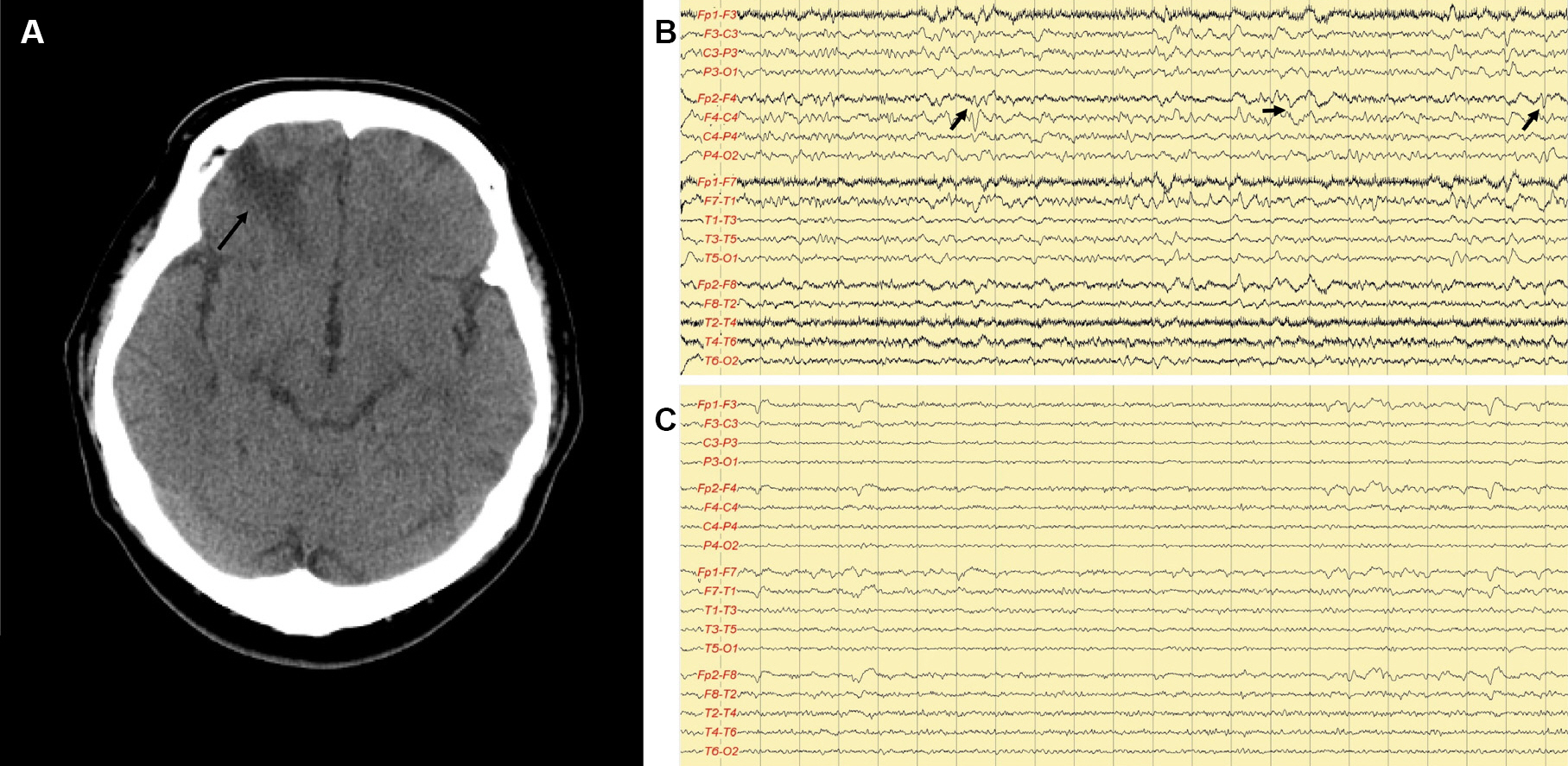
After that, he had no more seizures. However, about 3 weeks after cessation of the last seizure, he developed abnormal mood and behavioral symptoms, showed daily aggressive behavior toward his mother, and frequently expressed sexual desire to a female caregiver for whom he had sexual delusions. He responded irritably to the com-mands of medical personnel. The symptoms gradually worsened over the course of 1 month. Follow-up EEG revealed the disappearance of preexisting epileptiform discharges (Fig. 1C). At that time, he was alert and remembered those episodes.
He was referred to the Department of Psychiatry, where he was diagnosed with unspecific psychosis and mood disorder. His abnormal mood and behavioral symptoms gradually subsided after treatment with quetiapine 25 mg per day, haloperidol 1.5 mg per day, and escitalopram 10 mg per day. We changed the anti-seizure regimen to topiramate 50 mg twice a day and lamotrigine 100 mg twice a day. He has had rare seizures (3 to 4 per years) and has been free of psychiatric symptoms with anti-seizure and psychiatric treatment over the 10-year follow-up period.
Discussion
Psychiatric comorbidities, including mood, anxiety, and psychotic disorders, are common in PWE. They can be classified into preictal, interictal, and postictal disorders.1,3 Mood and psychotic disorders are usually explained as having a bidirectional relationship with epilepsy.1 Interictal and postictal psychiatric symptoms are commonly observed in clinical practice. However, psychiatric symptoms that develop after seizure remission in PWE are rare.
The existence of the phenomenon of FN remains in dispute since its first description by Landolt.2 The symptoms may be ascribed to the potential adverse effect of certain anti-seizure medications, long-term postictal psychiatric disorder, or genetic predisposition for mood or psychotic disorders of the patient.4 Possible mechanisms of FN include continuing epileptic status in the limbic system, propagation of epileptiform discharges along unusual pathways, and a role of anti-seizure medications in influencing the occurrence of sleep withdrawal and psychoses.5,6 Wolf proposed that epilepsy is still active in the subcortical area with active inhibitory processes, which lead to diverse psychiatric symptoms such as insomnia, hypervigilance, and mood instability.6 Another postulated mechanism is that amygdaloid and limbic kindling may be involved in developing this phenomenon.4,5,7 The antagonism between seizures and psychosis mediated by catecholamines has been demonstrated in kindling experiments. In contrast to epilepsy, gamma-aminobutyric acidergic (GABAergic) preponderance and glutaminergic deficit appear to be responsible for the pathogenesis of psychosis.4,5,8 Alterations in the balance of glutaminergic and GABA activity may cause seizures or behavioral disorders, and complex dopamine interactions may be involved in the development of FN.4,5
The criteria for FN diagnosis were: 1) diagnosis of epilepsy supported by clinical history, EEG, and neuroimaging; 2) acute/subacute behavioral disturbances; 3-1) reduction in the total number of epileptiform abnormalities counted in a 60 minutes awake EEG recording by over 50% compared to a similar recording performed during a normal state of behavior; 3-2) the absence of seizures for at least 1 week corroborated by a relative or caregiver. The supportive criteria for FN diagnosis were: 1) recent change in the drug regimen; 2) similar behavioral disturbances corroborated by a relative, caregiver, or general practitioner.8 To diagnose FN, it is necessary to identify primary criteria 1, 2, and 3-1 or primary criteria 1, 2, and 3-2 and one supportive criterion. The clinical findings in our patient met the criteria for FN (primary criteria 1, 2, and 3-1).
Certain anti-seizure medications, such as ethosuximide, vigabatrin, levetiracetam, and topiramate, may be related to the development of FN.8,9 Patients with sleep disturbances and previous psychiatric illnesses are reportedly vulnerable.8,9 FN is rarely reported in children and adolescents.10 A previous case report indicated that medication changes could help in the remission of the phenomenon.8
There is a possibility that psychosis could be a side effect of medication since FN often occurs after an effective anti-seizure medication is added. EEG improvement can be regarded as an epiphenomenon.11
The phenomenon of FN is a rare clinical manifestation. However, the exact pathological mechanisms remain to be elucidated. Unlike postictal psychosis or mood disorders, the symptoms last long after the cessation of seizures. Complete seizure remission may be a risk factor for the development of FN. Diagnoses can be made using clinical and electrographic methods. Changing the regimen of anti-seiz-ure medications and long-term psychiatric treatment may help control this phenomenon.